Filter
2997
Filtered Results: 2997
Text search:
Minister
of
Health
Featured
Recommendations
186
New Publications
952
Language
Document type
No document type
1818
Studies & Reports
534
Guidelines
236
Strategic & Response Plan
154
Manuals
107
Fact sheets
46
Situation Updates
45
Training Material
28
Infographics
11
Resource Platforms
8
Brochures
6
Videos
3
Online Courses
1
Countries / Regions
Congo, Democratic Republic of
118
Global
115
India
97
South Africa
96
Ethiopia
93
Nigeria
81
Liberia
78
Uganda
76
Sierra Leone
74
Myanmar / Burma
73
Senegal
70
Rwanda
69
Ghana
62
Zambia
55
Western and Central Europe
54
Africa
51
Namibia
50
Burkina Faso
48
Haiti
46
Nepal
45
Ukraine
44
Indonesia
44
Kenya
43
Tanzania
43
Cameroon
40
Benin
36
Bangladesh
35
Guinea
34
Syria
31
Eastern Europe
31
Malawi
30
Lesotho
28
Madagascar
27
Latin America and the Carribbean
25
West and Central Africa
25
Cambodia
23
South Sudan
23
Zimbabwe
21
East and Southern Africa
20
Mozambique
19
Asia
19
South–East Asia Region
18
Mali
18
Venezuela
17
Eswatini/ Swaziland
17
Afghanistan
15
Central African Republic
15
Middle East and North Africa
14
Côte d’Ivoire / Ivory Coast
14
Togo
12
Niger
12
Thailand
11
Yemen
11
Pakistan
11
Russia
10
Botswana
10
Germany
9
Vietnam
9
Somalia
9
Eastern Europe and Central Asia
8
Moldova
8
Sudan
8
Chad
8
China
7
Albania
7
Laos
7
Tajikistan
6
Peru
6
Philippines
6
Jordan
6
Lebanon
6
Colombia
5
Turkey
5
Burundi
5
Western Pacific Region
5
North Macedonia
4
Timor Leste/ East Timor
4
Papua New Guinea
4
Brazil
4
Sri Lanka
4
Palestine
4
Poland
4
Libya
4
Iraq
4
Mexico
3
El Salvador
3
Congo-Brazzaville
3
Italy
3
Hungary
3
France
3
Angola
3
Bhutan
3
Gambia
2
Kazakhstan
2
Iran
2
Canada
2
Malaysia
2
Morocco
2
Bulgaria
2
Mauritania
2
USA
2
Lithuania
2
Paraguay
2
North America
2
Japan
2
Mauritius
2
Spain
2
Israel
2
Bosnia and Herzegovina
2
Southern Africa
2
Argentina
2
Romania
2
Slovakia
2
Greece
2
Georgia
2
Honduras
2
Guatemala
2
Chile
1
Fiji
1
Singapore
1
Estonia
1
Kyrgyzstan
1
Uzbekistan
1
Armenia
1
Dominican Republic
1
Guinea-Bissau
1
Croatia
1
Ireland
1
Saudi Arabia
1
Denmark
1
Maldives
1
Tunisia
1
United Kingdom
1
Portugal
1
Bolivia
1
Belize
1
Costa Rica
1
Panama
1
Nicaragua
1
Egypt
1
Ecuador
1
Authors & Publishers
Publication Years
Category
Countries
1571
Public Health
129
Key Resources
124
Clinical Guidelines
107
Women & Child Health
100
Capacity Building
12
Pharmacy & Technologies
8
Toolboxes
COVID-19
212
HIV
156
Mental Health
151
TB
117
Ebola & Marburg
110
Disability
102
AMR
94
Rapid Response
84
Planetary Health
81
Conflict
79
Refugee
55
NTDs
55
Caregiver
53
Health Financing Toolbox
53
Global Health Education
51
Malaria
46
Natural Hazards
41
Pharmacy
31
Polio
25
NCDs
24
Cholera
23
Social Ethics
17
Specific Hazards
8
Zika
5
Typhoon
3
The COVID-19 pandemic is having a major impact on the mental health of populations in the Americas. Studies
show high rates of depression and anxiety, among other psychological symptoms, particularly among women, young
people, those with pre-existing mental health conditions, health workers, and p...
This guidance document is designed to ensure that the process of iteratively managing the health risks of climate change is integrated into the overall National Adaptation Planning (NAP) process, including through assessing risks; identifying, prioritizing, and implementing adaptation options; and m...
This survey is part of a series of eight country surveys conducted in the context of the People that Deliver Initiative (peoplethatdeliver.org). This global initiative, which brings together the world’s largest organizations, aims to improve health services performance through the professionalizat...
WAHA International’s mHealth programme addresses several barriers to maternal and neonatal care, including: a lack of information at the community level about locally available services; a large distance from services and a lack of affordable transport for patients; and ineffective communication b...
Introduction : de nos jours, face à la pénurie grandissante de
personnel de santé qualifié et face au défi de l’atteinte des
Objectifs du Millénaire pour le Développement, la participation
communautaire est devenue une réalité incontournable. Dans
la zone sanitaire Avrankou Adjarra Ak...
The present National action plan on antimicrobial resistance (AMR) with component of antimicrobial consumption (AMC) covering both human and agriculture sectors was developed based on the World Health Organization's (WHO) Global plan on AMR dated 2015. With the purpose to develop this plan, in May 2...
Ethiopia has been repeatedly affected by conflict, flooding, drought, and disease outbreaks in the past years. As of January 2024, the country is actively responding to the longest recorded cholera outbreak which started in August 2022, recurrent measles outbreaks which started in August 2021, and t...
A THESIS SUBMITTED IN PARTIAL FULFILMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER IN PUBLIC HEALTH OF THE UNIVERSITY OF NAMIBIA
This report describes findings from a telephone survey with 1,316 people conducted in February 2021. The survey examined how people respond to public health and social measures (PHSMs) to prevent COVID-19. The sample is representative of households with access to a landline or cell phone, but does n...
This report describes findings from a telephone survey with 1,328 people conducted in February 2021. The survey examined how people respond to public health and social measures (PHSMs) to prevent COVID-19. The sample is representative of households with access to a landline or cell phone, but does n...
Rehabilitation in health systems provides recommendations for Member States and other relevant stakeholders to strengthen and expand the availability of quality rehabilitation services. Currently, there is a significant unmet need for rehabilitation services and it is frequently undervalued in the h...
The purpose of this article is to consider the relationshipbetween religion and healthcarein order to suggest how physicians and other health care providers shouldrespond when the faith-based preference of apatient clashes with the medically indicatedtreatment modalities.
The COVID-19 Table-Top Exercise (TTX) is a simulation package which uses a progressive scenario together with series of scripted specific injects to enable participants to consider the potential impact of an outbreak in terms of existing plans, procedures and capacities. The aim of the TTX is to st...
Climate-related disasters, heatwaves, climate-sensitive diseases, and severe droughts and floods are taking lives and harming health, livelihoods, and ecosystems across the countries of the Caribbean, as in other Small Island Developing States (SIDS) around the world. In recognition of the high vuln...
This paper was commissioned by N´weti and Wemos as part
of the project “Equitable health financing for a strong health
system in Mozambique”. Its purpose is to contribute to the
debate of the Mozambican Ministry of Health’s draft Health
Sector Financing Strategy (HSFS) 2025 – 2034
Situational Analysis: 13-23 October 2014
Report prepared using the WHO/SEARO workbook tool for undertaking a situational analysis of medicines in health care delivery in low and middle income countries
Report prepared using the WHO/SEARO workbook tool for undertaking a situational analysis of medicines in health care delivery in low and middle income countries
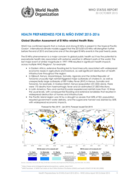
The WHO report on health preparedness for El Niño 2015-2016 describes the impact of this weather phenomenon on global public health. Strong El Niño events lead to extreme weather conditions, including droughts, floods, and storms, which increase the risk of diseases such as cholera, malaria, and d...
Non-Wood Forest Products 11
Traditional medicine and its use of medicinal plants is dependent on reliable supply of plant materials. The book focuses on the interface between medicinal plant use and conservation of medicinal plants.
Sectors in which Priority Adaptation Projects should be implemented first include:
- 1) Agriculture, Early Warning Systems and Forest (First Priority Level Sectors). This is followed by:
- 2) Public Health and Water Resources (Second Priority Level Sectors);
- 3) Coastal Zone (Thir...
- 1) Agriculture, Early Warning Systems and Forest (First Priority Level Sectors). This is followed by:
- 2) Public Health and Water Resources (Second Priority Level Sectors);
- 3) Coastal Zone (Thir...
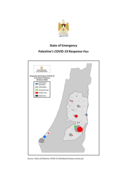
The purpose of this plan is to:
Present the GoP’s strategy and actions;
Propose an aid coordination approach;
Identify the critical support needs, including for: public health response to COVID-19; budget support to maintain government services; and diplomatic engagement with region...