Filter
400
Text search:
HIV
coinfection
Featured
50
106
Language
Document type
247
56
52
10
9
8
7
6
2
1
1
Countries / Regions
18
17
16
15
13
10
8
7
7
6
6
6
6
6
6
6
6
5
5
4
4
4
4
4
4
3
3
3
2
2
2
2
2
2
2
2
2
2
2
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
Authors & Publishers
Publication Years
Category
147
53
7
6
6
5
4
Toolboxes
128
94
28
8
7
6
3
3
2
2
2
2
1
1
1
1
1
1
The purpose of this guide is to provide updated clinical guidance on TB/HIV, with an emphasis on diagnostic aspects—including new techniques—as well as current treatment, while maintaining a public health approach. By compiling and consolidating
...
Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents With HIV K-19 Tuberculosis/HIV Coinfection
Updated: September 12, 2024 K
...
Volumen 5 / Número 1 , 1025-1028 • http://www.revistabionatura.com
To describe the behavior of Tuberculosis/Human Immunodeficiency Virus co-infection in a cohort of people affected by sensitive Tuberculosis in Ecuador from 01 January 2010 to 31 December 2015. Results: The percentage of co
...
Technical Update
Areas of Africa endemic for Buruli ulcer (BU), caused by Mycobacterium ulcerans, also have a high prevalence of human immunodeficiency virus (HIV), with adult prevalence rates between 1% and 5% (Maps). However, there is limited inf
...
Malaria and HIV, two of the world’s most deadly diseases, are widespread, but their distribution overlaps greatly in sub-Saharan Africa. Consequently, malaria and HIV
...
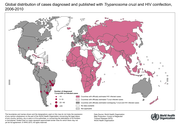
BMC Infectious Diseases Volume 25, article number 1289, (2025)
The boundaries and names shown and the designations used on this map do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its fro
...
BMC Pregnancy Childbirth 20, 379 (2020). https://doi.org/10.1186/s12884-020-03064-x
The leishmaniases are a group of diseases caused by Leishmania spp., which occur in cutaneous, mucocutaneous and visceral forms. They are neglected tropical diseases (NTDs), which disproportionately affect marginalized populations who have limited access to health care.
...
The emergence of SARS-CoV-2 has significantly altered the epidemiology of other infectious diseases, making investigations into its co-infection with malaria particularly relevant in endemic regions. This review examines the epidemiological, incubation and clinical features of the two diseases, high
...
Frontiers in Pediatrics | www.frontiersin.org
1 April 2019 | Volume 7 | Article 159
The checklist and reference list has two parts: high-level cross-cutting content (Part A) and specific programme content (Part B). Part A applies to all countries and contains situation and response analysis, the NSP development process, the goal, targets and priority-setting of the NSP and the prin
...
Topics in Antiviral Medicine, volume 33 Issue 2 May 2025
HIV & AIDS Treatment in Practice No. 188
Epidemiology
Chagas disease (American trypanosomiasis) is caused by the protozoan parasite Trypanosoma cruzi, and transmitted to humans by infected triatomine bugs, and less commonly by transfusion, organ transplant, from mother to infant, and in rare instances, by ingestion of contaminated food or
...