Filter
5371
Filtered Results: 5371
Text search:
health
profile
Featured
Recommendations
405
New Publications
1434
Language
Document type
No document type
3025
Studies & Reports
885
Guidelines
702
Manuals
223
Strategic & Response Plan
206
Fact sheets
129
Situation Updates
86
Training Material
61
Resource Platforms
24
Infographics
18
Brochures
6
Dashboards/Maps
4
Online Courses
2
Countries / Regions
India
227
Global
202
Kenya
141
Indonesia
136
Ethiopia
118
South Africa
102
Nepal
99
Nigeria
96
Western and Central Europe
94
Uganda
92
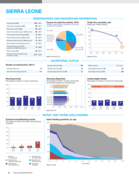
Sierra Leone
90
Rwanda
83
Myanmar / Burma
83
Latin America and the Carribbean
79
Africa
76
Bangladesh
74
Zambia
70
Ghana
68
Congo, Democratic Republic of
67
Senegal
66
Malawi
66
Tanzania
66
Namibia
66
Liberia
66
Ukraine
57
Philippines
51
Haiti
49
Brazil
48
Burkina Faso
46
Eastern Europe
46
Mozambique
45
Paraguay
45
Lesotho
44
Syria
44
Zimbabwe
42
Russia
40
Benin
37
Cambodia
37
Venezuela
36
Cameroon
34
Botswana
30
Asia
26
Colombia
25
Madagascar
25
Guinea
24
Germany
24
Eswatini/ Swaziland
24
South–East Asia Region
21
Argentina
21
South Sudan
21
Pakistan
21
Eastern Europe and Central Asia
19
East and Southern Africa
19
Yemen
18
Afghanistan
16
West and Central Africa
16
Togo
15
Bolivia
13
Somalia
13
Central African Republic
12
Thailand
11
Middle East and North Africa
11
Sudan
11
Angola
10
Ecuador
10
Tajikistan
9
Jordan
9
Iraq
9
Chile
8
Burundi
8
Lebanon
8
Moldova
8
Albania
7
Laos
7
Peru
7
Western Pacific Region
7
Côte d’Ivoire / Ivory Coast
7
Sri Lanka
7
Georgia
7
Guinea-Bissau
6
China
5
Niger
5
North America
5
United Kingdom
5
Belarus
5
Vietnam
5
Papua New Guinea
5
Egypt
5
Chad
5
North Macedonia
4
Timor Leste/ East Timor
4
Mexico
4
Turkey
4
Gambia
4
Iran
4
Estonia
4
Kyrgyzstan
4
Morocco
4
Armenia
4
USA
4
Romania
4
Palestine
4
Poland
4
Mali
4
Libya
4
Switzerland
3
Hungary
3
Saudi Arabia
3
Portugal
3
Spain
3
Southern Africa
3
Nicaragua
3
Djibouti
3
Honduras
3
Guatemala
3
El Salvador
2
Kazakhstan
2
Qatar
2
Italy
2
Jamaica
2
Maldives
2
Azerbaijan
2
Israel
2
Bosnia and Herzegovina
2
Greece
2
Australia
1
Canada
1
Singapore
1
Congo-Brazzaville
1
Mongolia
1
Bulgaria
1
Mauritania
1
Dominican Republic
1
Croatia
1
Ireland
1
Gabon
1
Uruguay
1
Turkmenistan
1
Denmark
1
Belgium
1
Tunisia
1
Norway
1
Latvia
1
Belize
1
Costa Rica
1
Panama
1
Bhutan
1
Authors & Publishers
Publication Years
Category
Countries
2502
Clinical Guidelines
387
Key Resources
271
Public Health
243
Women & Child Health
224
Capacity Building
66
Pharmacy & Technologies
42
Toolboxes
Mental Health
380
COVID-19
376
TB
343
HIV
331
Planetary Health
162
NTDs
155
AMR
146
Disability
139
NCDs
116
Conflict
106
Caregiver
103
Refugee
87
Rapid Response
86
Global Health Education
86
Ebola & Marburg
84
Pharmacy
82
Malaria
76
Natural Hazards
53
2.0 Rapid Response
48
Health Financing Toolbox
40
Zika
31
Cholera
29
Polio
25
Specific Hazards
13
Social Ethics
12
Promoting health and well-being throughout Europe
salud pública de méxico / vol. 50, suplemento 2 de 2008, pp.167-177.
In response to the emerging global concern regarding health and people with intellectual disabilities (ID), several developed countries have established national initiatives to address the unique health needs of this population ...
Ghana's attempt to regulate health care waste management started in 2002 with the development of guidelines on health care waste manage-ment by the Environmental Protection Agency (EPA). In 2006, the Ministry of Health developed the health care waste policy and guidelines. This guidance document im...
Int. J. Environ. Res. Public Health 2018, 15(12), 2626; https://doi.org/10.3390/ijerph15122626
Climate change is increasing risks to human health and to the health systems that seek to protect the safety and well-being of populations. Health authorities require information about current associatio...
Over the past decade, countries in the African region experienced slow progress in mobilizing resources for health while facing continued challenges. In their revised estimates published in 2017, Stenberg et al., developed two costs scenarios, termed progress and ambitious, aimed at strengthening co...
The government of Rwanda conducted the 2010 Rwanda Demographic and Health Survey (RDHS) to gather up-to-date information for monitoring progress on healthcare programs and policies in Rwanda, including the Economic Development and Poverty Reduction Strategy (EDPRS), the Millennium Development Goals ...
The Report describes the evaluation of WHO's contribution to the Maternal Health Program in South-East Asia Region. This was an independent evaluation conducted in 2015 by Amaltas, a Delhi based organization. The evaluation highlights the progress in five countries, namely Bangladesh, Indonesia, Mya...
Camp profile focused for the effective and efficient coordination
at camp level; continuity of service monitoring as per the
minimum or sectors’ standard; care and maintenance of the
service provisions; and immediate future planning for bridging
the gaps.