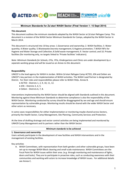
Filter
7634
Filtered Results: 7634
Text search:
facility
Featured
Recommendations
729
New Publications
2203
Language
Document type
No document type
4254
Guidelines
1173
Studies & Reports
1034
Manuals
413
Strategic & Response Plan
282
Fact sheets
171
Training Material
149
Situation Updates
65
Infographics
31
Resource Platforms
21
Brochures
18
Online Courses
17
Videos
4
Dashboards/Maps
1
App
1
Countries / Regions
India
411
Kenya
270
Global
242
Sierra Leone
201
Ethiopia
195
South Africa
189
Nepal
182
Liberia
178
Nigeria
175
Uganda
175
Rwanda
141
Malawi
140
Zambia
131
Tanzania
130
Latin America and the Carribbean
123
Bangladesh
117
Ghana
113
Namibia
100
Africa
95
Myanmar / Burma
92
Congo, Democratic Republic of
90
Western and Central Europe
88
Syria
83
Mozambique
78
Philippines
69
Senegal
61
Zimbabwe
55
Brazil
55
Ukraine
54
Cambodia
54
Burkina Faso
53
Lesotho
50
West and Central Africa
49
Venezuela
44
East and Southern Africa
44
South Sudan
44
Paraguay
43
Guinea
42
Haiti
41
Cameroon
39
Indonesia
39
Colombia
38
Middle East and North Africa
38
South–East Asia Region
38
Botswana
37
Russia
36
Asia
34
Yemen
34
Eastern Europe
33
Benin
29
Eswatini/ Swaziland
28
Peru
25
Germany
25
Central African Republic
24
Mali
24
Angola
23
Pakistan
22
Afghanistan
20
Western Pacific Region
19
Eastern Europe and Central Asia
19
Chile
17
Argentina
17
Bolivia
15
Somalia
14
Madagascar
14
Sudan
13
Vietnam
12
Ecuador
12
Jordan
11
Lebanon
11
Chad
11
Thailand
10
Laos
10
Niger
10
USA
10
Côte d’Ivoire / Ivory Coast
10
El Salvador
9
Iraq
9
Tajikistan
8
Burundi
8
Guinea-Bissau
8
Turkey
7
Portugal
7
Sri Lanka
7
Libya
7
China
6
North America
6
Mexico
5
Togo
5
France
5
Spain
5
Southern Africa
5
Moldova
5
Guatemala
5
Timor Leste/ East Timor
4
Gambia
4
Albania
4
Saudi Arabia
4
Papua New Guinea
4
Greece
4
Palestine
4
Georgia
4
Iran
3
Armenia
3
Turkmenistan
3
Tunisia
3
Bhutan
3
North Macedonia
2
Kazakhstan
2
Fiji
2
Singapore
2
Kyrgyzstan
2
Uzbekistan
2
Italy
2
Croatia
2
Gabon
2
Jamaica
2
Mauritius
2
United Kingdom
2
Algeria
2
Egypt
2
Romania
2
Poland
2
Switzerland
1
Serbia
1
Australia
1
Canada
1
Congo-Brazzaville
1
Malaysia
1
Morocco
1
Mongolia
1
Qatar
1
Bulgaria
1
Mauritania
1
Hungary
1
Lithuania
1
Ireland
1
Japan
1
Denmark
1
Maldives
1
South Korea
1
Israel
1
Guyana
1
Solomon Islands
1
Authors & Publishers
Publication Years
Category
Countries
3597
Clinical Guidelines
504
Key Resources
452
Women & Child Health
440
Public Health
297
Capacity Building
204
Pharmacy & Technologies
78
Toolboxes
COVID-19
880
HIV
458
TB
458
Mental Health
288
Caregiver
264
Ebola & Marburg
260
AMR
213
Rapid Response
212
Disability
188
Conflict
180
Planetary Health
153
Pharmacy
150
NTDs
140
Refugee
97
Malaria
96
Natural Hazards
88
Health Financing Toolbox
84
NCDs
72
Global Health Education
71
Cholera
56
Polio
41
Specific Hazards
40
Zika
21
Social Ethics
9
Typhoon
3
A guide to promote health systems strengthening to achieve universal health coverage.
Guidelines for Critical Care of Seriously Ill Adult Patients with Coronavirus (COVID-19) in the Americas
recommended
Short Version
This clinical practice guideline was developed in order to provide recommendations for the management of critically ill adult patients with COVID-19 in intensive care units (ICUs).
In Tanzania, institutional efforts to combat HIV/AIDS started in 1985 by establishing a National Taskforce within the Ministry of Health. This was so because the HIV/AIDS epidemic was first perceived as a health problem, and the initial control efforts were formulated and based within the health sec...
This interim guidance is aimed at assisting organizers of international meetings attended by individuals from EVD-affected countries and individuals with a travel history to EVD-affected countries within the previous 3 weeks.
The first part is intended for organizers of international meetings, to ...
The Councils share a common mandate of ensuring persons practising health related professions in Namibia are suitably qualified. Registration with the Councils is, thus, a pre-requisite for professional practice – and it is also a legal requirement too update personal details of all registered hea...
Senegal’s substantial and sustained progress against malaria is an inspiring public health success story, and a source of potential lessons for other countries on the path to elimination. This case study describes three major success factors—(1) outstanding leadership and partner engagement, (2)...
Tuberculosis cases, TB deaths
Int J Tuberc Lung Dis. 2019 Jul 1;23(7):858–864.Namibia ranks among the 30 high TB burden countries worldwide. Here, we report results of the second nationwide anti-TB drug resistance survey. To assess the prevalence and trends of multidrug-resistant TB (MDR-TB) in Namibia.
From 2014 to 2015, pat...
Strategy for Increasing the use of Modern Contraceptives in Nigeria