Filter
1817
Filtered Results: 1817
Text search:
Mobilität
Featured
Recommendations
149
New Publications
569
Language
Document type
No document type
1089
Studies & Reports
236
Guidelines
191
Strategic & Response Plan
125
Manuals
84
Fact sheets
33
Training Material
25
Situation Updates
17
Brochures
7
Infographics
7
Resource Platforms
3
Countries / Regions
Congo, Democratic Republic of
120
Senegal
104
Indonesia
75
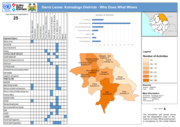
Sierra Leone
63
Benin
61
Burkina Faso
61
India
49
Global
46
Guinea
42
Uganda
41
Nigeria
39
Africa
37
Kenya
36
Zambia
36
Haiti
34
Nepal
32
Central African Republic
32
Mali
32
Liberia
32
South Africa
30
Malawi
28
Rwanda
26
Brazil
25
Ghana
23
Madagascar
23
Cameroon
22
Ethiopia
22
Namibia
21
Mozambique
20
West and Central Africa
20
Côte d’Ivoire / Ivory Coast
17
Togo
16
Myanmar / Burma
16
Tanzania
15
Niger
14
Lesotho
13
Zimbabwe
12
Latin America and the Carribbean
12
East and Southern Africa
12
Bangladesh
11
Western and Central Europe
10
Syria
9
Paraguay
9
Chad
8
Botswana
8
Cambodia
7
Germany
7
Angola
7
Burundi
6
South Sudan
6
Pakistan
6
Ukraine
5
Venezuela
5
Eswatini/ Swaziland
5
Peru
4
Asia
4
Guinea-Bissau
4
Middle East and North Africa
4
Portugal
4
Eastern Europe
4
Colombia
3
Timor Leste/ East Timor
3
South–East Asia Region
3
Spain
3
Vietnam
3
Sudan
3
Yemen
3
Somalia
3
Ecuador
3
Tajikistan
2
El Salvador
2
Serbia
2
China
2
Congo-Brazzaville
2
Morocco
2
Philippines
2
Croatia
2
France
2
Mauritius
2
Bolivia
2
Sri Lanka
2
Russia
2
Guatemala
2
North Macedonia
1
North Korea
1
Switzerland
1
Gambia
1
Chile
1
Iran
1
Kyrgyzstan
1
Afghanistan
1
Mauritania
1
Jordan
1
North America
1
Turkmenistan
1
Japan
1
Maldives
1
Azerbaijan
1
Bosnia and Herzegovina
1
Southern Africa
1
Lebanon
1
Papua New Guinea
1
Moldova
1
Egypt
1
Romania
1
Poland
1
Bhutan
1
Iraq
1
Authors & Publishers
Publication Years
Category
Countries
970
Key Resources
107
Women & Child Health
71
Clinical Guidelines
68
Public Health
57
Capacity Building
22
Pharmacy & Technologies
7
Toolboxes
COVID-19
170
Ebola & Marburg
138
Disability
75
Mental Health
67
HIV
55
Rapid Response
53
Malaria
53
TB
52
NTDs
42
Planetary Health
37
Conflict
31
Refugee
28
Caregiver
27
Natural Hazards
25
AMR
23
2.0 Rapid Response
20
Cholera
19
Global Health Education
18
Health Financing Toolbox
17
Polio
11
Zika
8
Pharmacy
6
NCDs
4
Typhoon
4
Specific Hazards
2
Social Ethics
2
Le "Plan Stratégique National de Communication pour le Changement Social et de Comportement en Lutte contre le Paludisme" de la République Démocratique du Congo (RDC) vise à renforcer les actions de prévention et de traitement du paludisme à travers un changement social et comportemental. Ce p...
This chapter of the AMP LLIN Mass Campaign Toolkit outlines the strategic communication approaches that are essential before, during and after long-lasting insecticide-treated net (LLIN) distribution campaigns. It emphasises the importance of setting up a national communications sub-committee under ...
La Stratégie nationale de communication pour le paludisme 2017–2020 de la République Démocratique du Congo vise à améliorer les comportements de prévention, de détection et de traitement du paludisme à travers une communication sociale et comportementale (CSC) structurée et contextuelle. ...
Le Plan Stratégique National de Lutte contre le Paludisme de la RDC vise à renforcer la communication pour le changement social et comportemental (CSC/CCC) dans la lutte contre le paludisme. Il a pour objectif d’améliorer les connaissances, attitudes et pratiques des populations pour encourager...
RBM Partnership to End Malaria
recommended
The RBM Partnership to End Malaria is a global coalition comprising over 500 partners, including governments, international organisations, the private sector and civil society, who are all dedicated to ending malaria worldwide. Through coordinated advocacy, resource mobilisation and technical suppor...
Le Plan Stratégique National de Lutte contre le Paludisme 2023–2027 de la Guinée vise à réduire de 80 % l’incidence et la mortalité liées au paludisme d’ici 2027, en s’appuyant sur les leçons des années précédentes. Il prévoit des actions renforcées de prévention (moustiquaire...
Le Plan Stratégique National de Lutte contre le Paludisme 2021–2027 du Burundi expose la vision d’un Burundi sans décès lié au paludisme d’ici 2027. Le programme vise à réduire de 60 % la morbidité et à atteindre zéro mortalité grâce à une couverture universelle en prévention (m...
Le Plan Stratégique National de Communication pour le Changement Social et des Comportements en matière de Lutte contre le Paludisme 2021–2025 de la Côte d’Ivoire définit les grandes lignes pour améliorer la prévention et la prise en charge du paludisme à travers la communication. Il vise...
Le Plan Stratégique National de Lutte contre le Paludisme au Sénégal 2021–2025 a pour objectif de réduire l’incidence et la mortalité liées au paludisme d’au moins 75 % par rapport à 2019 et d’interrompre la transmission locale dans au moins 80 % des districts éligibles. Il repos...
En 2024, le Cap-Vert et l’Égypte ont été certifiés exempts de paludisme, ce qui prouve qu'il est possible d'éliminer la maladie avec une volonté politique et des ressources adaptées. Cependant, en Afrique, où se concentrent 95 % des cas mondiaux et 97 % des décès (en 2023), les progrès ...
The NDMS&IP focuses on mainstreaming disability to promote equitable access to services in the six thematic areas of health, education, livelihoods, empowerment, and social inclusion and cross-cutting issues.
The first part of the NDMS&IP outlines incongruences between national and sectoral policie...
Africa’s health sector is facing an unprecedented financing crisis, driven by a sharp decline of 70% in Official Development Assistance (ODA) from 2021 to 2025 and deep-rooted structural vulnerabilities. This collapse is placing immense pressure on Africa’s already fragile health systems as ODA ...
The overall goal of the programme, to reduce the malaria morbidity and mortality by 75% (using 2012 as baseline) by the year 2020, continued to be pursued in 2014. The following areas were identified as some of the priorities for the year: Malaria Case Management under which we have Malaria in Pregn...
Scaling Up Mental Health Care In Rural India