Filter
10655
Filtered Results: 10655
Text search:
Maske
Featured
Recommendations
905
New Publications
2572
Language
Document type
No document type
5777
Studies & Reports
1786
Guidelines
1263
Manuals
628
Strategic & Response Plan
333
Fact sheets
311
Training Material
257
Infographics
93
Situation Updates
69
Brochures
59
Resource Platforms
50
Videos
15
Online Courses
12
Dashboards/Maps
1
App
1
Countries / Regions
Global
491
India
481
Kenya
290
South Africa
241
Ethiopia
215
Sierra Leone
211
Uganda
192
Liberia
192
Nepal
190
Nigeria
189
Myanmar / Burma
174
Western and Central Europe
155
Bangladesh
150
Africa
145
Zambia
144
Rwanda
138
Tanzania
134
Malawi
133
Germany
133
Syria
130
Ghana
125
Latin America and the Carribbean
117
Namibia
96
Ukraine
89
Philippines
85
Congo, Democratic Republic of
80
South Sudan
68
Indonesia
68
Lesotho
62
Zimbabwe
62
Haiti
61
Cambodia
60
South–East Asia Region
59
West and Central Africa
52
Guinea
51
Asia
50
East and Southern Africa
49
Senegal
45
Yemen
45
Mozambique
43
Eastern Europe
43
Lebanon
41
Middle East and North Africa
40
Cameroon
36
Burkina Faso
35
Venezuela
35
Afghanistan
33
Botswana
33
Central African Republic
31
Pakistan
30
Colombia
26
Eswatini/ Swaziland
26
Brazil
25
Eastern Europe and Central Asia
24
Russia
23
Sudan
23
Somalia
23
Mali
22
China
21
Western Pacific Region
21
Vietnam
21
Thailand
20
USA
18
Jordan
18
Iraq
17
Laos
15
Sri Lanka
15
Benin
14
Turkey
13
Tajikistan
12
North America
12
Côte d’Ivoire / Ivory Coast
12
Albania
11
Chile
10
Peru
10
United Kingdom
10
Moldova
10
Southern Africa
9
Greece
9
Georgia
9
Togo
8
Iran
8
Libya
8
North Macedonia
7
Niger
7
Burundi
7
Paraguay
7
Jamaica
7
Chad
7
Ecuador
7
Madagascar
7
Kyrgyzstan
6
Palestine
6
Switzerland
5
Timor Leste/ East Timor
5
Mexico
5
Kazakhstan
5
Canada
5
Malaysia
5
Argentina
5
Papua New Guinea
5
Serbia
4
Gambia
4
Fiji
4
Guinea-Bissau
4
Portugal
4
Spain
4
Bolivia
4
Angola
4
Bhutan
4
El Salvador
3
Singapore
3
Italy
3
Armenia
3
Croatia
3
Turkmenistan
3
Japan
3
Egypt
3
Poland
3
Honduras
3
Australia
2
Estonia
2
Uzbekistan
2
Austria
2
Vanuatu
2
Morocco
2
Dominican Republic
2
Hungary
2
Lithuania
2
Ireland
2
Mauritius
2
Tunisia
2
South Korea
2
Azerbaijan
2
Belarus
2
French Guyana
2
Israel
2
Nicaragua
2
Guatemala
2
North Korea
1
Congo-Brazzaville
1
Mongolia
1
Qatar
1
Bulgaria
1
Mauritania
1
Saudi Arabia
1
Gabon
1
Denmark
1
Belgium
1
France
1
Maldives
1
Norway
1
Bosnia and Herzegovina
1
Latvia
1
Belize
1
Costa Rica
1
Panama
1
Romania
1
Solomon Islands
1
Authors & Publishers
Publication Years
Category
Countries
3760
Key Resources
722
Clinical Guidelines
665
Women & Child Health
583
Public Health
547
Capacity Building
274
Pharmacy & Technologies
89
Annual Report MEDBOX
3
Toolboxes
COVID-19
974
Mental Health
839
HIV
730
Disability
536
Planetary Health
400
TB
388
Caregiver
322
Refugee
308
Conflict
308
Ebola & Marburg
305
NTDs
269
AMR
244
NCDs
183
Global Health Education
180
Rapid Response
170
Pharmacy
169
Natural Hazards
160
Health Financing Toolbox
150
Malaria
107
2.0 Rapid Response
103
Social Ethics
98
Cholera
87
Specific Hazards
74
Zika
56
Polio
55
Typhoon
9
South Sudan
2
To help parents keep their children healthy and fit, WHO has developed the Child Nutrition and Physical Activity Guide. In addition to parents, the guide may prove to be a useful tool for other adults (such as grandparents or caregivers) working with primary school-aged children.
The Child Nutrit...
A general consensus exists that as a country develops economically, health spending per capita rises and the share of that spending that is prepaid through government or private mechanisms also rises. However, the speed and magnitude of these changes vary substantially across countries, even at simi...
On Global Handwashing Day, WHO and UNICEF have released the first-ever global Guidelines on Hand Hygiene in Community Settings to support governments and practitioners in promoting effective hand hygiene outside health care – across households, public spaces and institutions. Framing hand hygiene ...
Version 02, veröffentlicht am 23.12.2020
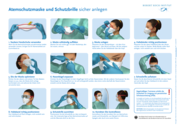
Atemschutzmaske und Schutzbrille sicher anlegen
recommended
This report is the first of its kind. It brings together various data sets to present the current status of hand hygiene, highlight lagging progress, and call governments and supporting agencies to action, offering numerous inspiring examples of change.
During the COVID-19 pandemic, hand hygiene ...
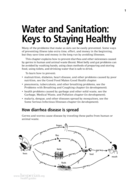
This content is from the Advance Chapters of the NEW Where There Is No Doctor
Novel Coronavirus (COVID-19)
Accessed: 08.04.2020
Evaluation report
December 2014
Health educators have been advocating for the inclusion of climate and environmental education in medical and nursing curriculums for the past two decades. BMJ 2021;375:n2385 http://dx.doi.org/10.1136/bmj.n2385 Published: 06 October 2021